Continuing our Future of Work series, we’re going to take a look at an industry that has been on the front lines of this pandemic, healthcare. The spotlight on this industry segment during this time has resulted in everything from praise and support to jeers and even threats. Healthcare professionals are going through a lot of the same stress and strain that all of us are right now, but they also have the additional stress of providing and/or supporting those who are sick in the middle of a pandemic. However, even with all the stress they’re under, there are some signs that point to the possibility of a bright future for the people who make our healthcare industry.
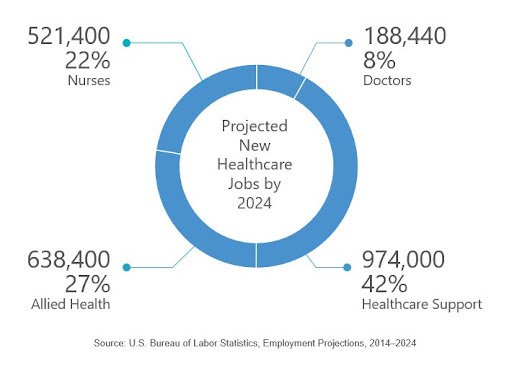
Even before COVID-19 impacted the United States, the healthcare industry was facing some tough challenges. One of those challenges was the result of projections around the number of new healthcare workers needed in the future. The Bureau of Labor Statistics (BLS) projected that 2.3 million new nurses, doctors, healthcare support and allied healthcare workers would be needed by 2024, which is faster growth than any other employment sector. The drivers of these projections are that people have longer life expectancies, technological advances, healthcare reforms and the aging Baby Boomer population. That last driver (aging Baby Boomers) is also a factor that’s driving the shortage of healthcare workers.
More Baby Boomers need healthcare, but they’re also all reaching the age of retirement, which means more people are vacating their healthcare jobs than there are people to replace them. Information in the 2018 and 2019 reports from the Association of American Medical Colleges (AAMC) provides a good picture of future healthcare needs. Specifically, by 2032, the U.S. expects to have a shortage of 46,900 to 121,900 doctors. For every five physicians who are working, two will be over the age of 65 and ready for retirement. And even more immediate is that by 2020, almost half of all nurses will be due for retirement. Knowing this, 90% of healthcare executives have stated that they actively worry about being able to fill essential healthcare positions.

And now that the pandemic is taking place, some of those healthcare workers are facing even more than just the virus. For instance, recall that a large portion of people working in healthcare are from an aging population and information is presenting evidence that over a quarter of current healthcare workers are at increased risk of contracting COVID-19 due to age and other health factors. Additionally, this research has found that many of the healthcare workers on the frontline of the pandemic have family incomes that are below the poverty line, which includes 2.5% of hospital workers. And 275,000 healthcare workers in direct patient contact are uninsured, and the 1.12 million healthcare workers who are at risk of bad COVID-19 outcomes don’t have paid sick leave. Finally, many healthcare workers have had a terrible time getting the proper personal protective equipment (PPE) and have even had to resort to reusing PPE that is meant to be disposed of, or even fashioning PPE out of materials like trash bags.
An additional stressor healthcare workers are facing is related to the security of their jobs and those of their coworkers. Intuitively, one might think that the healthcare sector would be relatively safe from layoffs and furloughs. However, those on the frontline of the healthcare industry are watching as their coworkers in other departments are being furloughed, often related to restrictions on non-COVID-related illness and the reduction of elective surgeries. A Google search for “healthcare furlough” produces numerous articles across the nation showing huge numbers of workers who are being furloughed or facing pay cuts. And in fact, on April 29, 2020, the U.S. announced that the GDP for the country contracted by 4.8% and healthcare services a sharp 2.3% contraction in relation to overall GDP.
As we start to look to the future of the healthcare industry, there’s a lot to consider. Given what existing healthcare workers have been through, there’s a strong chance that those still in the field may face a great deal of disillusionment with their career choices. Of those who watch their coworkers be furloughed or laid-off, 74% report that they experience a form of “survivor’s guilt” and suffer from productivity loss. Being threatened with termination for not putting your life at risk using improper PPE or reporting these violations is defined as a “toxic workplace culture.” These workplace cultures can cause workers to leave their jobs and even shift to a different career path in extreme cases. So, it is possible that the shortages identified by the AAMC may be exacerbated by even more healthcare workers abandoning their careers due to their experiences during the COVID-19 pandemic. Hopefully, as we move forward from this, regulatory agencies and government commissions will react to the conditions that healthcare workers have labored under and there will be a renewed focus to bolster and improve their working conditions, PPE shortages and protections. In fact, recent steps are underway to consider forgiving student loans for these frontline healthcare workers. So, with this as a good beginning, there may be even more efforts in the future to address the challenges faced by these workers and create incentives for them to remain a part of the industry.
There are existing recruiting pipeline models used by healthcare providers prior to the pandemic that could be used on a large scale to impact the shortages that exist. For example, Hawai’i Pacific Health faces an even more complex shortage challenge than other states. Due to their location in the middle of the Pacific ocean, they’re unable to easily recruit workers from nearby states. So, their shortages have been more extreme than the rest of the U.S. To address shortages of medical assistants, nurse aides and surgical instrument processing technicians, Hawai’i Pacific Health partners with high schools to begin identifying students with an interest in and an aptitude for healthcare. While these students are still in high school, they are provided with classes to teach them the basic skills for the jobs they are interested in, and upon graduation, they are immediately offered employment.

Another program that could be used to great effect post-pandemic is the program used by Mercy Health – West Michigan. Mercy Health developed a powerful Evidence-Based Selection Process (EBSP) that allows them to hire faster and more efficiently in a tight labor market. They then work closely with local community colleges and their local workforce agency, West MichiganWorks!, to create a regional talent pipeline. Essentially, their community partners are using the same tools that Mercy Health would use to “pre-wire” candidates with a career portfolio that would better prepare them for the first steps into a healthcare career with Mercy Health. Using talent pipelines in this way could help healthcare systems direct candidates into their recruiting pool while they are still students, vastly increasing hiring rates. Tools that support skills-based hiring, like PAIRIN Hiring, can be particularly helpful in identifying young talent who have the right skills to perform specific jobs in specific industries and settings, such as healthcare.
One change to the current healthcare experience has been a dramatic drop in the number of in-person patient visits, leading to the need to look carefully at how patients engage with the healthcare industry. A great number of people have started to use telemedicine, which is seeing your doctor through your phone, tablet or computer instead of an in-office visit. Prior to the pandemic, the use of telemedicine was limited to relatively minor complaints. However, many people are using telemedicine much more often, and the healthcare industry has responded by expanding the types of patient needs that can be addressed through this medium and will likely work even more to innovate better solutions in the future. This is similar to how the banking industry made drastic changes in how customers managed their financial needs. Twenty years ago, if you needed to make a simple deposit, you had to go into a bank and speak to a teller. Now, even complex loans and mortgages are handled using technology, requiring no in-person bank visits. Additionally, we may even see the usage of artificial intelligence to bolster and support the work of specialists such as anesthesiologists, nurses and health technologists.
Healthcare right now is tough. It’s probably one of the toughest professions to be in, and frankly, some people may choose to move on. But those who choose to stay will be an extremely passionate, caring and committed group of professionals that will help move our healthcare system into the future. And, with the recent microscope on the vast healthcare needs, the industry is well-positioned to benefit from future innovations and solutions to tackle the challenges they are facing now. We’ll build a stronger, better world for healthcare workers and patients, and we’ll be ready for the next challenge.
Stay with us as we move to our fourth blog in this five-part blog series, where we will explore the field of delivery and logistics and how it has changed from a service most may not have thought about much, to an essential backbone of our society – both now and in the future. Then we’ll close out the series looking at the field of tech and IT to discover how it’s been pushed to its limits and where it might go to in the future, touching every aspect of work to provide new and exciting career opportunities.
